Insulin is a vital hormone that plays a central role in regulating the metabolism of carbohydrates, fats, and proteins in the human body. Produced by the pancreas, insulin is essential for maintaining blood glucose levels and ensuring that cells receive the energy they need for proper functioning. In this article, we will explore the pivotal role of insulin in body metabolism and the implications of its dysfunction.
Insulin’s Key Functions:
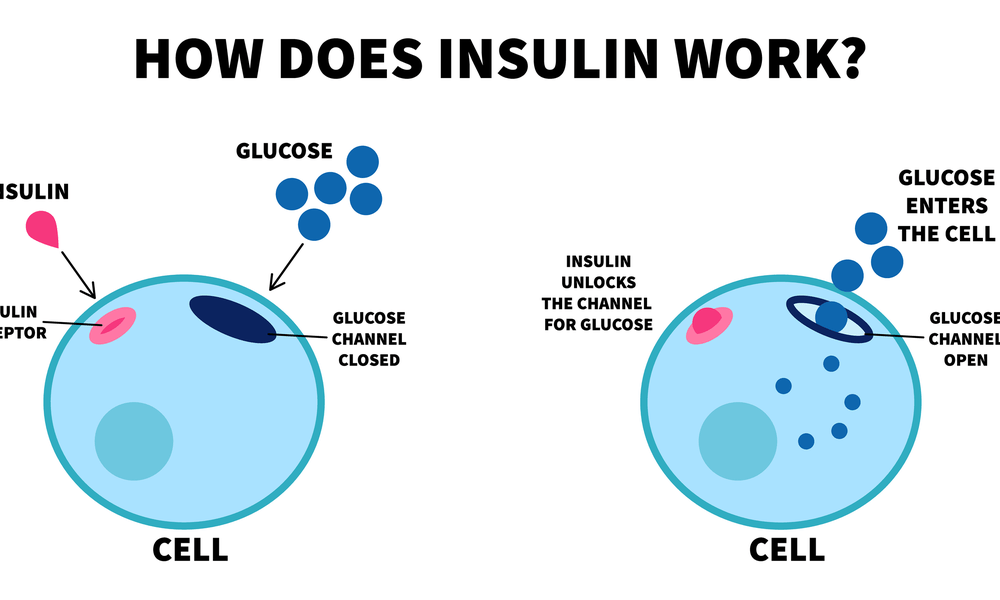
Regulating Blood Glucose: One of insulin’s primary functions is to regulate blood glucose levels. When you eat, especially foods high in carbohydrates, your blood sugar rises. Insulin is released into the bloodstream to facilitate the uptake of glucose by cells, reducing blood glucose levels.
Energy Storage: Insulin promotes the storage of excess glucose in the liver and muscles in the form of glycogen. This stored energy can be readily converted back into glucose when needed.
Lipid Metabolism: Insulin regulates the metabolism of fats (lipids) by promoting the uptake of fatty acids and inhibiting their release from fat cells. It also encourages fat storage and prevents excessive fat breakdown.
Protein Metabolism: Insulin facilitates the uptake of amino acids, the building blocks of proteins, by cells. This is vital for protein synthesis, muscle growth, and tissue repair.
Cellular Uptake: Insulin helps transport glucose and other nutrients into cells. This process ensures that cells have the necessary energy and building blocks for their various functions.
Implications of Insulin Dysfunction:
- Diabetes Mellitus: Dysfunction of the insulin system is a hallmark of diabetes mellitus. There are two primary types of diabetes:
Type 1 Diabetes: This autoimmune condition results in the destruction of the insulin-producing beta cells in the pancreas. People with Type 1 diabetes require external insulin to manage their blood sugar levels.
Type 2 Diabetes: In Type 2 diabetes, the body becomes resistant to the effects of insulin, and the pancreas may not produce enough insulin to compensate. Lifestyle factors, genetics, and obesity are often associated with Type 2 diabetes. Management involves lifestyle modifications, medications, and, in some cases, insulin therapy.
- Metabolic Syndrome: Insulin resistance is a key component of metabolic syndrome, a cluster of conditions that increase the risk of heart disease, stroke, and type 2 diabetes. Other components of metabolic syndrome include high blood pressure, abnormal cholesterol levels, and abdominal obesity.
- Obesity: Insulin resistance and elevated insulin levels can contribute to obesity. Excess insulin promotes fat storage, making it harder for the body to utilize stored fat for energy.
Insulin is a critical hormone that regulates various aspects of body metabolism. Its role in maintaining blood glucose levels and facilitating the uptake of nutrients by cells is essential for overall health. Dysfunction of the insulin system, as seen in diabetes and metabolic syndrome, has significant implications for health and requires careful management. Understanding the importance of insulin in metabolism underscores the need for a balanced and healthy lifestyle to support its optimal functioning.